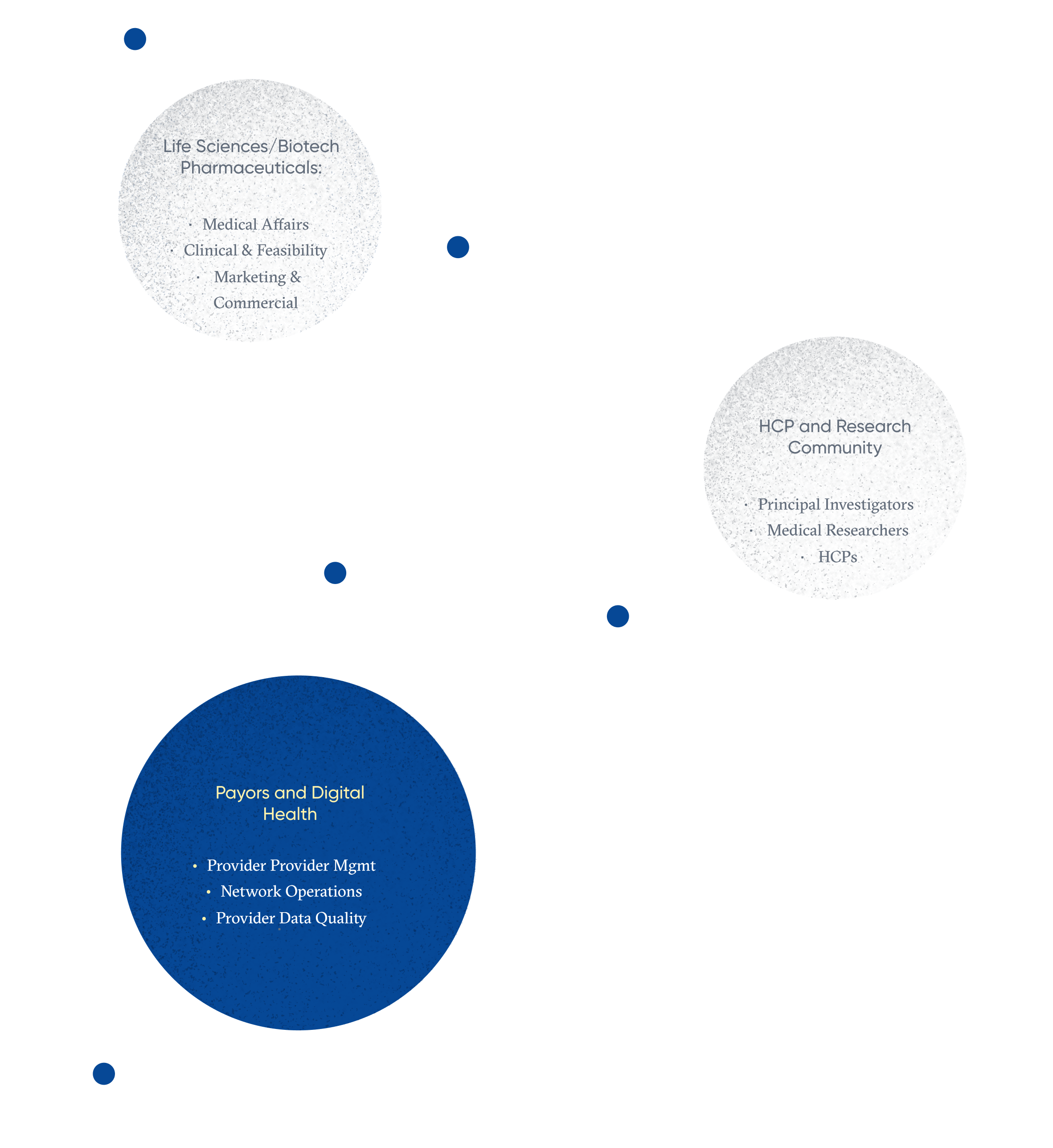
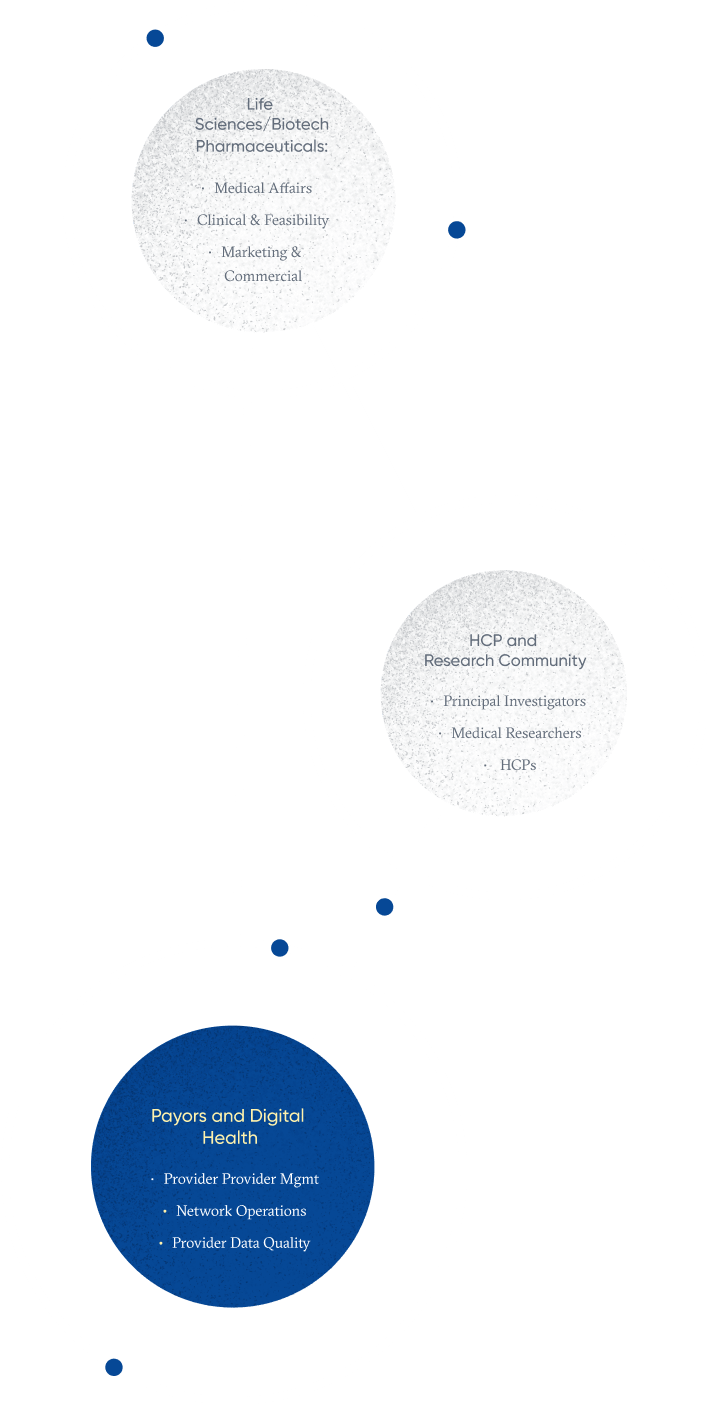
Payors and Digital Health
Transforming provider data quality and patient access
Payors have the responsibility of improving efficacy, quality, and cost of care in addition to ensuring patients have access to the right healthcare professionals at the right time.
Data is at the center of their efforts. Unfortunately the data payors depend on is often siloed and outdated, leaving them exposed to fines and operational inefficiency, and leaving their members at a disadvantage.
Accurate information is also necessary to meet the Triple AIM framework, a three-pronged approach focused on improving the patient experience, reducing the per capita costs of healthcare, and improving the health of populations overall. Achieving Triple AIM is also crucial to the success of healthcare organizations moving toward value-based care payment systems. Building adequate, high-quality provider networks and ensuring patients utilize in-network resources is all part of the big picture.
However, provider data is particularly challenging to maintain. Aggregated, disambiguated, and validated data is the backbone of H1’s offerings. Our provider data management ecosystem continuously monitors for data inaccuracies for fast resolution. We vet and maintain demographic provider data, active state licensing, patient coverage, affiliation, office hours, and data from additional sources to help patients and payors alike have access on demand to the most accurate repository possible.
Use Cases
Address requirements set forth by regulations like H.R. 133, the Interoperability and Patient Access Rule, and the No Surprises Act (NSA), which protects patients from unauthorized out-of-network billing.
Maintain accurate and balanced provider networks that adequately address patient volume and need across therapeutic areas.
Reduce administrative processes and reduce costly errors when referring patients to in-network providers.
Meet regulations like H.R. 133, the Interoperability and Patient Access Rule and the No Surprises Act (NSA) with confidence.
We improve provider data quality and patient access to an equitable healthcare system.
How We Help
Provider data collection requirements are becoming increasingly more complex and require updating and confirming with greater frequency.
To improve accuracy, regulators have set minimum requirements for how frequently plans must contact practices to verify and update their information.
There’s a lot of overlap among the data sets required for directory maintenance. That is why streamlining provider data collection is critical to success. H1 takes the burden off of payors.
Provider Data Management
Access consistently accurate and properly maintained provider information.
Redefine the data standard for every U.S. provider.

Network Operations and HCP Recruitment
Streamline referral processes.
Recruit the right providers to meet the needs of members and patients.
Provider Data Quality
Reduce regulatory non-compliance exposure and fines.
Improve member experience and access to care.

Industry Benefits
Increased Member Satisfaction
Increased Member Satisfaction
Create a streamlined patient experience that delivers accurate, up-to-date contact information, affiliation data, license verification, and in-network healthcare insurance organizations’ and plans’ certification.
Optimized Provider Networks
Optimized Provider Networks
Maintain the right volume of doctors across specialties based on the needs of the patients you cover.
Reduced Penalties for Non-Compliance
Reduced Penalties for Non-Compliance
Mitigate fines associated with the No Surprises Act and other provider data quality regulations.
Streamlined Data Management and Provider Referral Operations
Streamlined Data Management and Provider Referral Operations
Automate manual data verification processes to lessen the burden on already taxed IT staff.
Trusted by over 250+ leading companies
Trusted by over 250+ leading companies







“Our partnership with H1 ensures expediency, data integrity, and compliance, so our members can optimize their care with the most up-to-date information in the fastest amount of time possible.”
Anirban Gangopadhyay| Co-founder and CTO of Angle Health