For Health Plans
Streamline provider data management to elevate your member experiences
Our leading provider data management platform enables healthcare organizations to automate highly manual data processing and build better member experiences.
Trusted by industry leaders


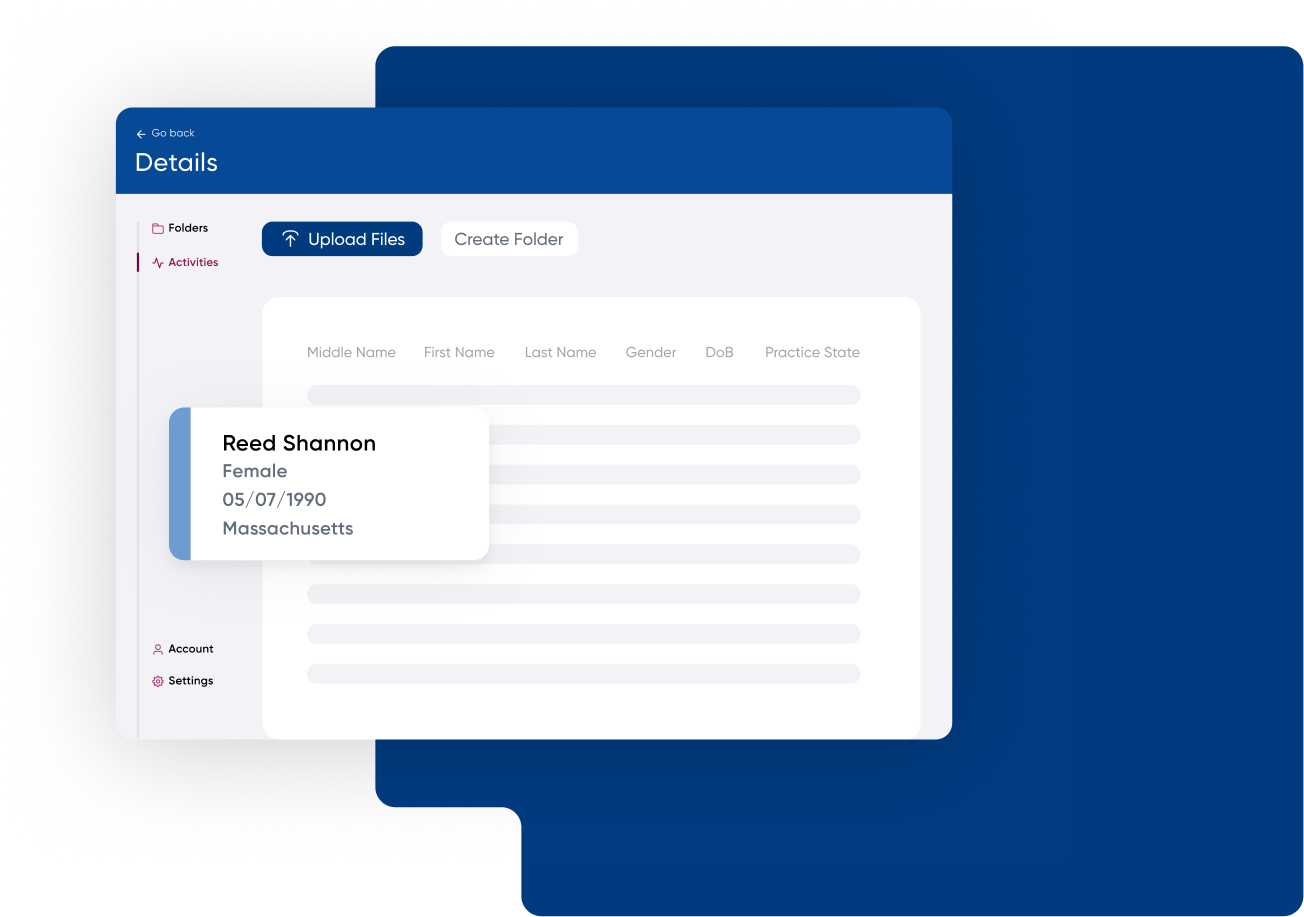
Our Provider Data Platform
Streamline your provider data workflows to achieve substantial time and cost savings while improving data quality and operational efficiency.
$0.30
PMPM cost reduction for health plans
90%
accuracy across provider directories
55%
reduction in member complaints
5x
more productivity in data management
Our solutions
Seamlessly integrate comprehensive provider data and intelligence into your existing systems and workflows.
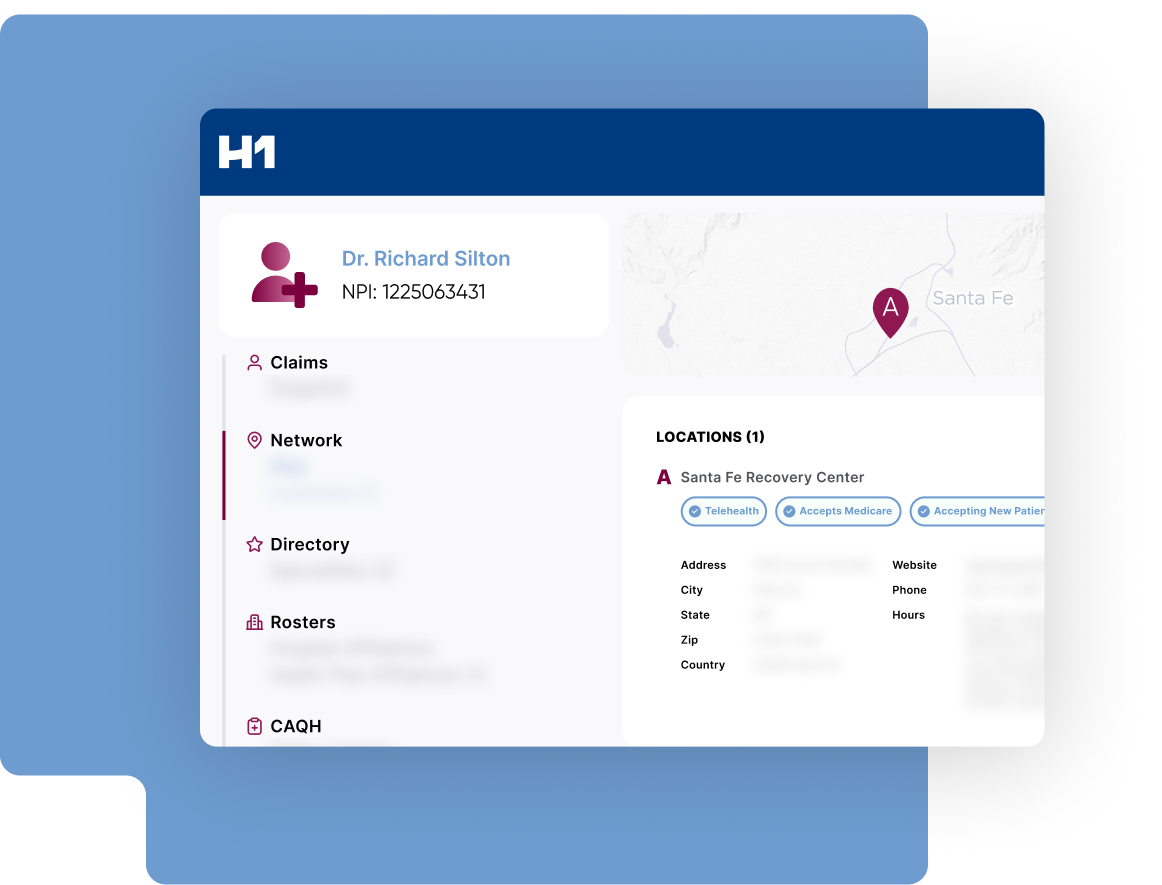
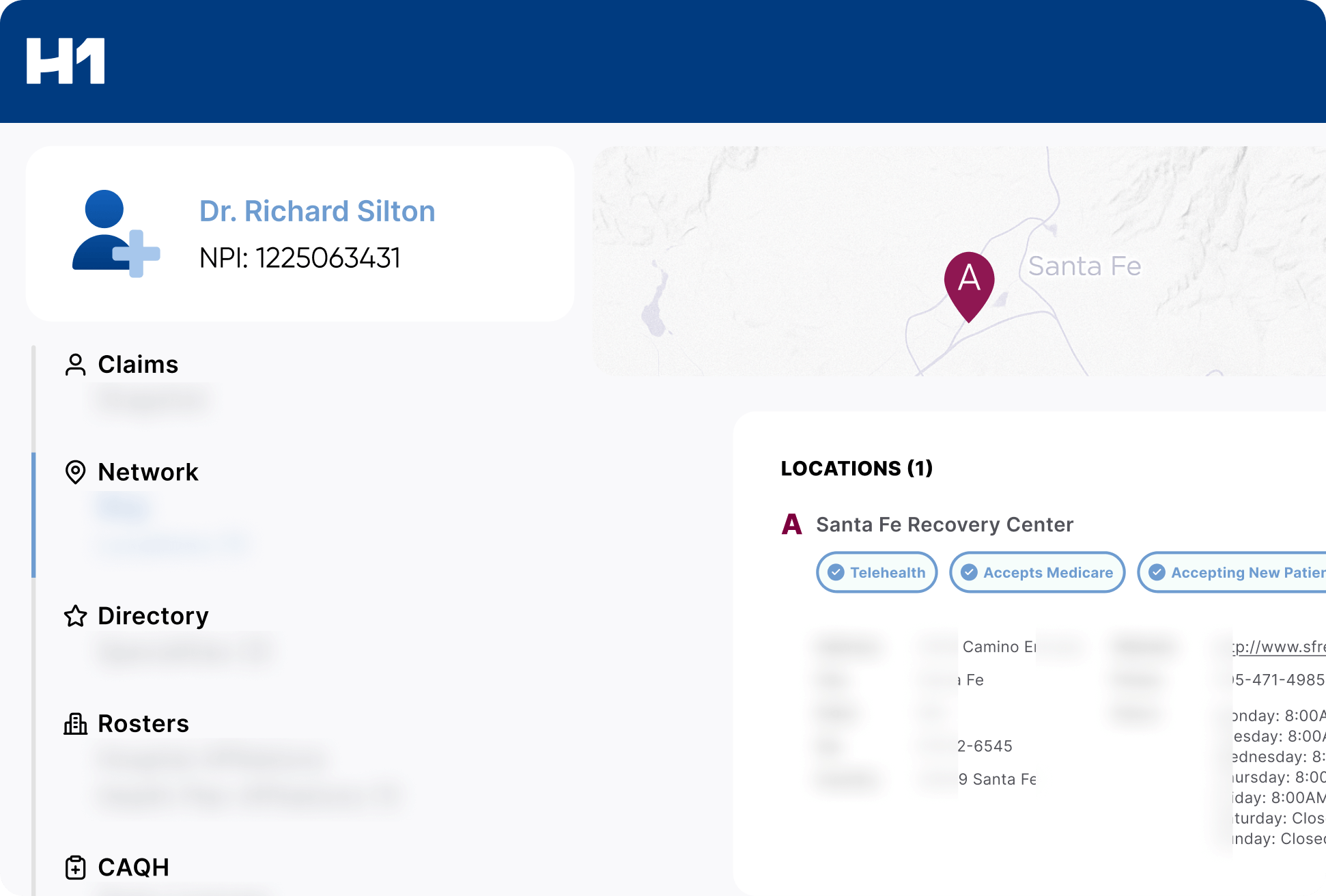
Provider Data Management
Transform fragmented provider data into a single source of truth. Our solution integrates all your provider data sources, assesses data quality with AI-powered Accuracy Scoring, implements automated data quality improvements at scale, and configures standardized data for use across your organization.
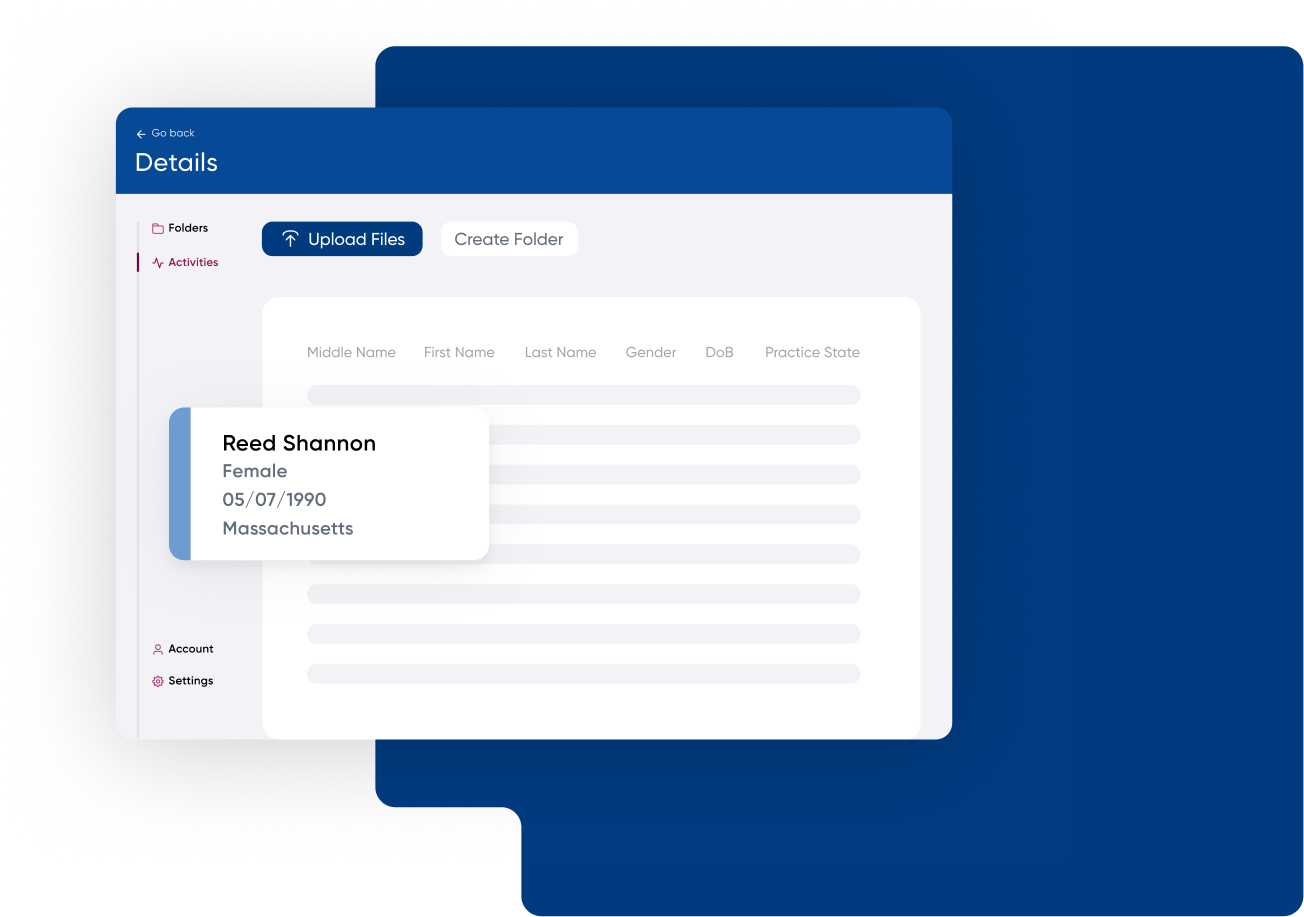
Roster Automation
Automate provider roster ingestion with our AI-powered solution. It formats, validates, and updates incoming rosters in minutes with over 90% accuracy, standardizing diverse formats and enhancing data. Streamline ingestion while effectively processing files and preventing bad data entry.
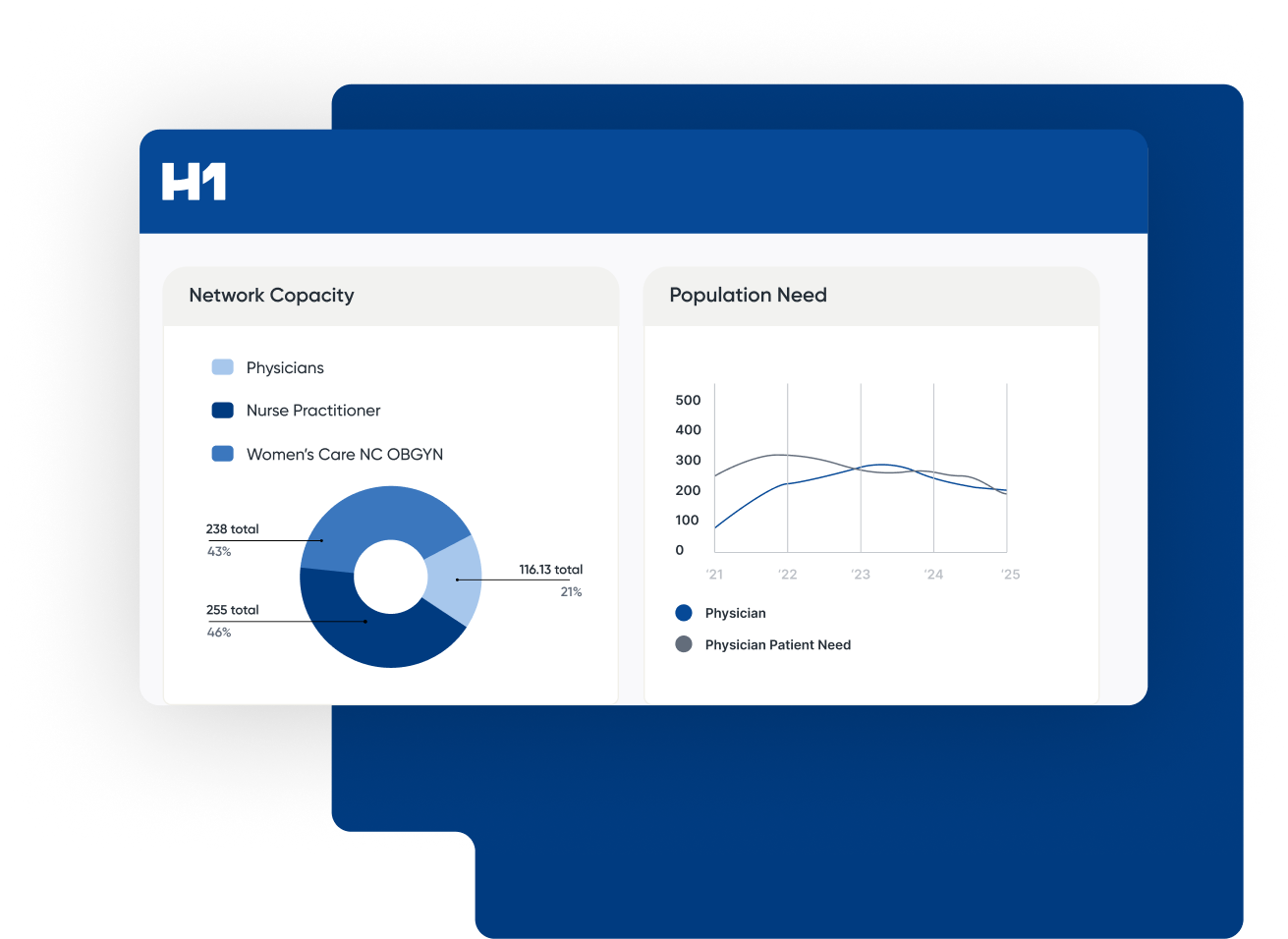
Network Analytics
Provides members with timely access to adequate in-network providers for high-quality care across diverse areas and populations. Find the right information about providers, groups, and facilities, whether building a new network, filling existing gaps, or developing new systems.
Directory Stream
Improve directory accuracy through AI-powered models that differentiate good and bad data at scale. Enrich provider information with comprehensive nationwide directory data covering 99.9% of NPIs and locations, building the most accurate and complete dataset.
Solving the provider data problem from every angle
Tailored provider data solutions for the critical downstream needs of healthcare organizations, transforming what was once an operational headache into a source of efficiency and business value.
Improve Directory Accuracy and Quality
Utilize H1’s AI-powered Accuracy Scoring technology to analyze, cleanse, and measurably improve your provider data.
Establish Provider Data ‘System of Record’
Use H1 as your core provider data hub to ingest all of your data sources, centralize and store data, execute updates at scale, and flexibly configure outputs across all sources.
Automate Roster Standardization
H1 ingests and standardizes rosters of different formats into one, normalized source of truth, and tracks changes over time.
Derive Network and Market Insights
Perform meaningful industry analyses, gain market intelligence, and optimize network design with H1 provider data.
Streamline Claims Processing
Optimize claims adjudication to ensure accurate physician payments, reducing errors and enhancing efficiency for health plans.
Support Regulatory Compliance
Meet specific directory accuracy and network adequacy requirements for Medicaid, Medicare, and Commercial plans.
“The primary decision-maker was that the product features, functionality, and breadth met all our needs by quite a margin over the second-place contender. And once we started to dig in with the team, they were super great to work with.”
VP of Product Management, National Health Plan